Bodily Changes You Can Expect While Pregnant pt. 2
Learn More
Bodily Changes You Can Expect While Pregnant
Learn More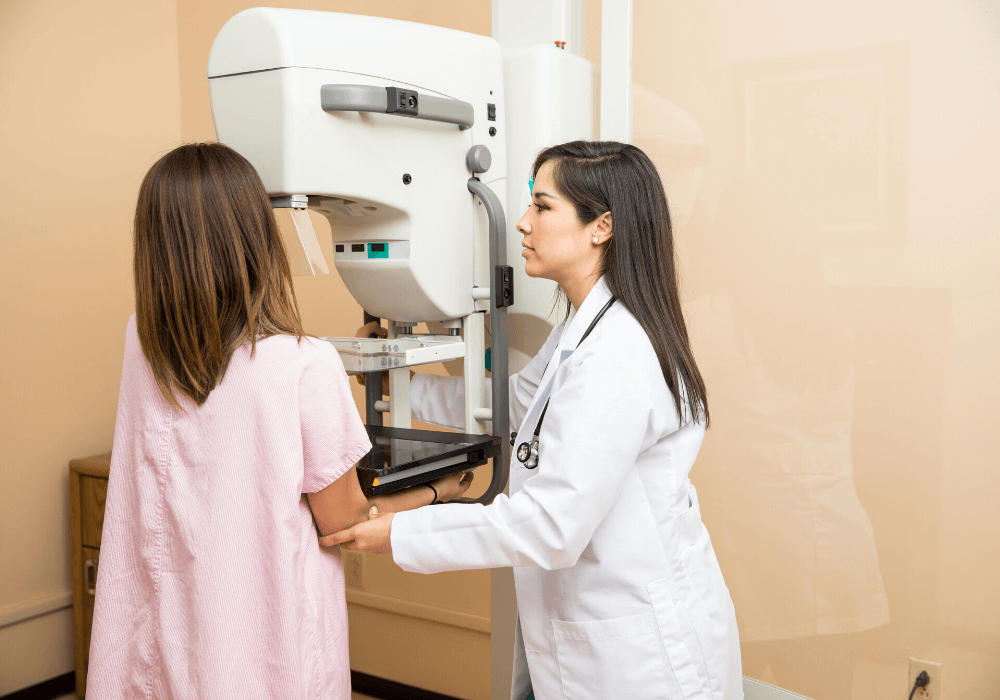
Everything You Need to Know About Mammograms
Learn More
What You Should Know About Birth Control
Learn More
Top 11 Foods to Avoid During Pregnancy
Learn More
Managing Stress During Pregnancy
Learn More
Health Benefits of Breastfeeding for Both Mom and Baby
Learn More
Why Acne During Pregnancy Is Common and How to Get Rid of It
Learn More